Established in the Affordable Care Act, the Hospital Readmissions Reduction Program (HRRP) aims to reduce the number of preventable 30 day readmissions— and the numbers have declined since its inception. In fact, the Kaiser Family Foundation notes that rates actually began to fall in 2012 as hospitals anticipated that penalties would be applied based on prior year performance, dropping by 8 percent nationally in the past few years.
Penalties for preventable readmissions could total $521 million
Still, the program is not without its detractors. J. Michael McWilliams, MD, PhD, associate professor of healthcare policy and medicine at Harvard Medical School and practicing internist at Brigham and Women’s Hospital in Boston, wrote in JAMA Internal Medicine that, “The readmissions reduction program is designed to penalize hospitals for poor quality of care, but our findings suggest that hospitals are penalized to a large extent based on the patients that they serve.”
If Readmissions Are Down, Why Are Penalties Up?
To the relief of many hospitals, one in four hospitals won’t face readmission penalties in 2023 as a result of COVID-19. But in 2021, the Centers for Medicare and Medicaid Services (CMS) announced that penalties for preventable readmissions could total $521 million because of changes in how readmissions are measured.
Since 2012, the CMS has expanded the list of covered conditions to include 30-day readmissions for:
- Heart attack
- Heart failure
- Pneumonia
- Chronic obstructive pulmonary disease (COPD)
- Coronary artery bypass graft surgery
- Elective total hip and total knee replacements
But additions to the covered conditions are not the only reason that some hospitals face higher penalties than others. So what are the top causes of 30-day readmissions?
Factors that Pose a Higher Risk of Readmission
1. Health Condition
Naturally, a patient’s health condition plays a role in readmissions. A study conducted by the Agency for Healthcare Research and Quality (AHRQ) on readmissions from 2018 identified septicemia as the top cause of readmissions among Medicare patients, followed by congestive heart failure, COPD, pneumonia and renal failure.
2. Insurance Type
The same study also found that a patient’s health insurance coverage also influenced readmissions. Readmissions were highest among Medicare patients at more than 16.9 percent. Next in line were Medicaid patients at 20.6 percent, while private health insurance patients accounted for 18.6 percent and uninsured patients a mere 4.9 percent. Researchers at Boston’s Beth Israel Deaconess Medical Center took a closer look at readmissions and concurred, noting that patients who had Medicare or Medicaid faced a higher risk of readmission within eight or more days after discharge.
3. Timing
By splitting readmissions into two categories — 8-day and 30-day — the researchers also uncovered some interesting trends:
- Patients readmitted within eight days were inclined to be experiencing complications from the original condition, while patients readmitted closer to 30 days after discharge were more likely to have lacked follow-up care or developed a new illness or complication.
- Patients discharged between 8 a.m. and 1 p.m. were less likely to be readmitted to the hospital, leading researchers to hypothesize that earlier discharge enabled patients and family caregivers to make arrangements for follow-up care or to pick up prescriptions.
So far, we’ve been looking at the clinical side of the issue, but what about the patients themselves?
4. Demographics & Psychographics
Numerous studies, including one published in the Journal of Healthcare Quality, have found that race, gender, age and income are good predictors of 30-day readmissions. For example, the study found that women treated for heart attacks were 17 percent more likely to be readmitted within 30 days. The study also found that patients in lower income communities faced higher readmission numbers than those in higher-income communities.
Upfront analyzed the psychographic segment distribution across issues related to hospital readmissions and found some provocative insights.
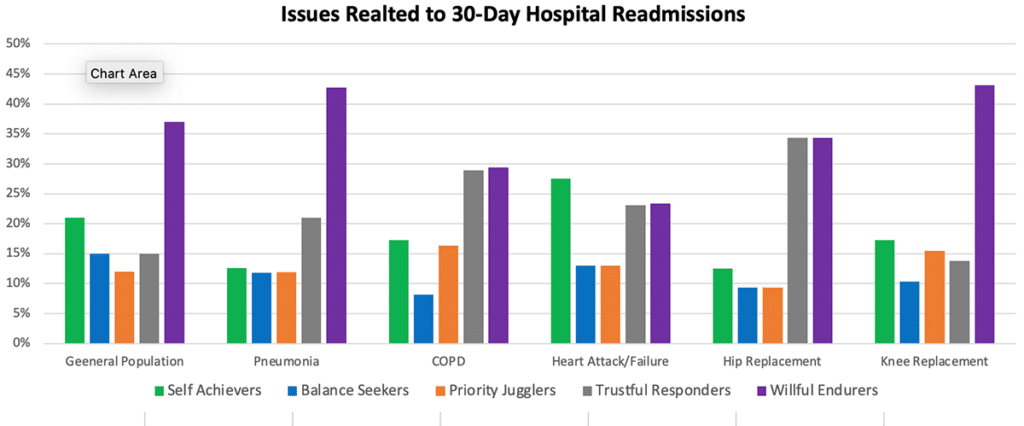
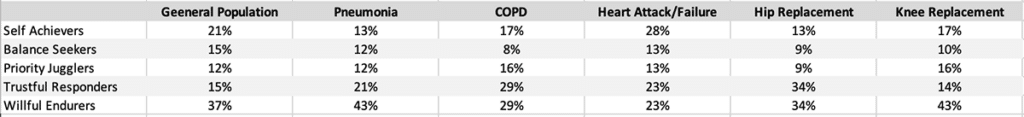
Willful Endurers — the segment that lives in the “here & now” and is generally disengaged with health and wellness until they absolutely have to address a health issue — represents 37 percent of the general population. However, among issues related to hospital readmissions, Willful Endurers are strongly over-represented. Willful Endurers are unique in their priorities and motivations and do not respond as well to typical healthcare education and communications. If a hospital wants to make significant improvements in its readmission rates, it needs to recognize the healthcare personalities of its patients and engage them accordingly.
5. Low Patient Engagement
Patient engagement can be influenced by demographic factors. For instance, ethnicity may result in language barriers that reduce engagement. Likewise, education and health literacy may frustrate engagement efforts.
How Patient Engagement Technology can Help Discharge Management
When you look at all of the factors that cause hospital readmissions, it’s clear that hospitals need to define clear strategies to manage the discharge process and engage patients. Hospitals tend to handle the discharge of patients based on broad characterizations — by diagnosis or by demographic segment, for example — with one-size-fits-all communications.
Instead, hospitals need to personalize their efforts to match patients’ unique motivations and attitudes related to health and wellness. Psychographic segmentation offers that level of insight, and when paired with an automated patient engagement and access platform like Upfront, hospitals can better understand what messages offer the relevance needed to support successful post-discharge recovery — from providing educational materials and recovery tracking to appointment reminders and medication adherence surveys.
While many suggest that the route to lower readmissions is better collaboration with providers outside hospital walls, it is also critical that such collaboration takes place with the patients themselves. Are you ready?



