The transformation of healthcare is accelerating. As patients demonstrate an open willingness to change providers at the drop of a hat in the pursuit of quality, affordable, and convenient care, healthcare enterprises are left scrambling to keep patients in the fold. Yet, returning to healthcare’s status quo is no longer a viable option.
On the heels of Amazon’s bold $3.9 billion acquisition of primary care company OneMedical, they have every reason to be concerned. In February, the ecommerce tech giant essentially jumped the line into local community healthcare systems, sending shockwaves across the industry as healthcare enterprises — still recovering from the grip of the pandemic — now also grapple with the acquisition’s impact.
Kaufman Hall reports a median year-to-date margin index at -1.1%, placing many healthcare systems effectively in the red.
Amazon isn’t alone, of course. CVS Health also announced its acquisition of Oak Street Health, solidifying the company’s footprint in value-based care.
Behind the scenes, these moves expose significant ramifications for shifting digital behaviors and attitudes in health. A recent national market research study conducted by Upfront Healthcare and Ipsos found that more than half of respondents under age 45 agree that “Amazon knows me better than my doctor knows me,” a sentiment that should sound the alarm for any healthcare executive looking to protect or grow their market share.
Putting personalization into play
Today’s healthcare consumers expect the same personalized customer experiences they encounter with familiar brands. Across industry sectors, McKinsey & Company found 71% of consumers expect companies to deliver personalized interactions, and 76% express frustration when this personalization doesn’t happen.
And with more care options on the table than ever before, patients express less patience when it comes to poor healthcare experiences. When a healthcare provider fails to meet their expectations, they’re apt to simply move on.
As providers find new ways to increase revenue stability, contain costs, and differentiate themselves, they are taking on more risk, which requires cohesive strategies to ensure patients feel empowered and supported in playing a larger role in their health.
It’s one of the reasons why healthcare enterprises are becoming more involved in not just providing care, but in identifying and proactively addressing the underlying social, structural, and societal drivers of health. To prevent net losses, healthcare enterprises need to deeply understand existing barriers to care, and then surface resources to patients when they need them most.
But when the pandemic struck, many organizations sought to stem patient leakage by investing in a range of patient engagement solutions — including self-scheduling tools and text messaging — without good patient insights. These “shot in the dark” attempts often resulted in technology fragmentation, underperformance, or downright failure.
At the same time, healthcare organizations were left scratching their heads trying to understand why they were not getting the engagement they expected from patients or “left on read.”
Here’s a reality check: Healthcare enterprises can no longer push patient engagement off to the sidelines or allow it to become an afterthought. It can’t be solved with a mass text message. And it certainly isn’t going to work until advanced personalization, a skill companies such as Amazon have already mastered, becomes a top strategic priority across the entire organization.
One-off campaign-based approaches or 'clickbait tactics' to connect with patients won’t work. Successful patient engagement requires easing access and augmenting in-person clinic visits with proactive digital communication in between visits to effectively build trust throughout the patient journey.
Lindsay Zimmerman
Vice President, Bartosch Patient Activation Institute

Healthcare consumption vs. care
Over the past few years, “healthcare consumerism” has become a buzzword flitting through patient engagement circles, as well as across the industry. The concept of healthcare consumerism is generally focused on using information and technology to help patients make more informed healthcare decisions. While this broad call-to-action for the healthcare community is a good one, especially with giant consumer-focused companies encroaching on the space, healthcare should be less about consumption — and more about care.
Sending mass text messages and simply crossing our fingers that patients will follow through isn’t enough to win their trust or stand against the competition. So, how can healthcare enterprises earn patient loyalty?
Deeply knowing your patients’ demographics, utilization patterns, social needs, and psychographic profiles — their behaviors, core motivations, preferences, and needs — provides a start. If we know a goal-oriented patient would value an appointment tomorrow, rather than schedule a visit with their PCP two months down the road, our ongoing, personalized communications should reflect that.
But, let’s be super clear. There is no silver bullet to patient engagement. It takes hard work, experimentation, and proven solutions to succeed. Let’s examine three areas healthcare leaders should consider while building their approach to a sustainable and resilient enterprise.
#1 Healthcare shouldn’t feel transactional. Trust is built through a series of micro-interactions.
It’s no secret that engaging patients is key to improving the value of care, yet healthcare enterprises continuously miss the mark on providing a positive patient experience. Roughly 2 in 3 patients report a poor patient experience, including poor communication with doctors, inefficient visits, surprise healthcare bills, murky medical advice, and a general lack of empathy or emotional support. To put it plainly, no patient wants to feel like a number.
One-off campaign-based approaches or “clickbait tactics” to connect with patients won’t work. Successful patient engagement will require easing access and augmenting in-person clinic visits with proactive digital communication in between visits to effectively build trust throughout the patient journey — for example, immediately post-discharge from an emergency department visit or before they are overdue for an annual wellness visit. Continuous support includes reaching out to patients during moments that matter.
#2 Health outcomes must be prioritized over vague engagement indicators.
Too often, healthcare enterprises gauge a program’s success on engagement indicators. The focus should be on patient activation. What’s the difference? Patient activation happens when patients recognize they play a key role in their healthcare and take action. When patients are activated, they are more likely to speak openly with their providers, actively track their health conditions, schedule preventative care and follow-up visits, and engage in healthier behaviors in their daily lives.
Healthcare systems, however, are simply measuring the wrong thing. Instead, patient outreach strategies should be designed and measured by the clinical, financial, and operational results set forth in strategic goal planning. For example:
- Number of patients who show up for care
- Reduction of no-shows
- Care gaps and readmissions
- Number of FTE hours diverted to higher-priority tasks
- Topline revenue growth
In Oncology care, health systems have used patient activation information to gauge patient sentiment, mental health, or even to predict diagnoses. While technology should be used to augment the patient experience, it should also be viewed as a means to a greater end.
#3 Successful patient activation requires cross-functional collaboration to achieve the ultimate goal: a cohesive, defragmented patient experience
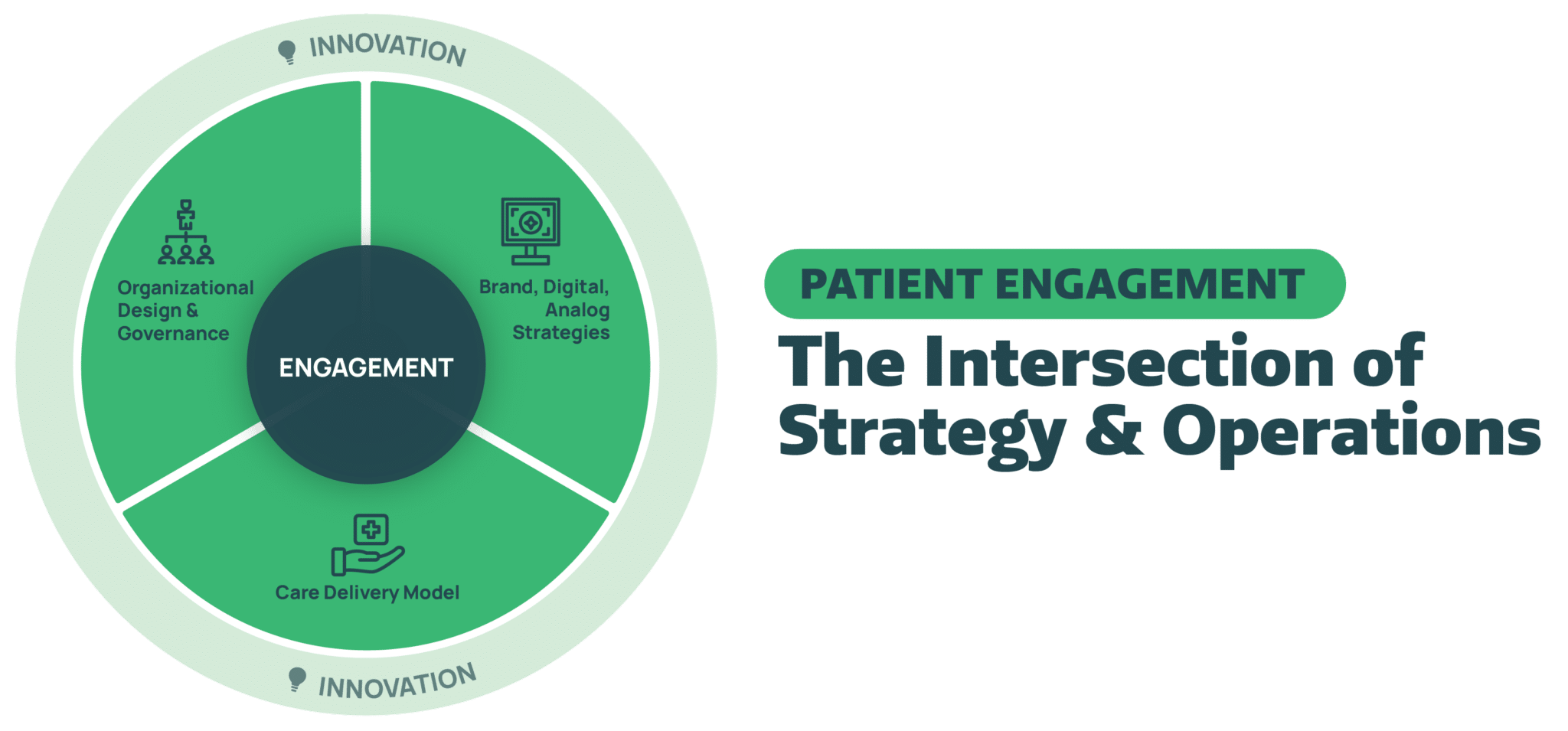
Healthcare organizations can’t think about patient engagement as a side project, but rather an organization-wide initiative sitting at the intersection of strategy and operations. Deploying a successful patient engagement program requires clear governance and the buy-in of stakeholders at every level, including IT, operations, the care delivery model, marketing, and more. This will eliminate silos that could impede a program’s success and ensure patient engagement initiatives reflect the broader brand, digital, and analog strategies of the healthcare organization.
The end goal of healthcare communication must be a cohesive, defragmented, and patient-oriented experience. Today, patients may receive dozens of messages a week – from various sources, channels, and point solutions – related to their health and healthcare. That leaves patients inundated by disparate messages and unclear, frustrated, and confused about what action to take next.
In a recent JAMA Internal Medicine article, Drs. Duckro & Steiner called out the main challenges with communication ecosystems in health care, and eloquently described what communication should look like:
“The goal of communication ecosystems in health care is to improve patient health, quality, safety, engagement, and efficiency of care. System-generated communications can help achieve these goals. A well-designed communication strategy may even help retain patients and attract new ones. To do so, healthcare systems must create a coherent, patient-centered strategy to develop and test their communications and harmonize a potential cacophony of solo voices into a well-orchestrated choir.”
Meeting complex healthcare challenges head-on
While many technology vendors promise magical digital solutions to motivate patients, the reality is engaging patients remains difficult work that must be driven by an applied behavioral design process: a systematic approach to understanding, and influencing, specific patient behaviors and outcomes. For example, many technology vendors celebrate contact rates as high as 97-99% but fail to mention visit adherence or scheduling rates following initial contact, which is often nowhere near those numbers. It’s an empty boast.
It’s also one of the reasons why we launched the Bartosch Patient Activation Institute, our applied research center that’s dedicated to solving complex healthcare challenges with evidence-based research, data insights, and design.
By fusing behavioral science with psychographics segmentation to create personalized patient experiences, healthcare enterprises can embrace consumer-centric strategies to win patients over and achieve positive patient activation outcomes.





